The Pain Matrix: What Pain Matrix?

INTRODUCTION
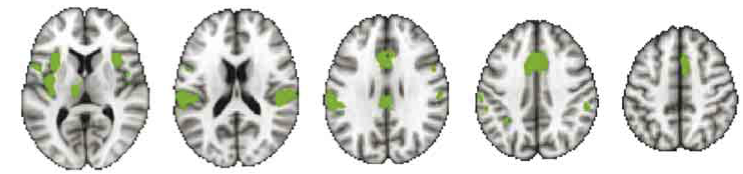
Since Melzack's brilliant proposal of a "neuromatrix" in the brain, much study has been devoted to imaging brain function in relation to pain. It was based on an idea from animals in which a question was: "What makes a deer, antelope or giraffe in the wild, stand up and start walking as soon as it can after birth? There must be a set of neurones (or matrix) that is programmed to produce actions that ensure the animal's survival." A corollary became: "Maybe a matrix in the brain that serves pain, a protective (or survival) strategy associated with threat." From Melzack's fantastic proposal spawned copious research into activity in parts of the brain when people have pain. A corollary of this was a belief that a pain matrix exists because there seemed to be common brain areas between studies that show activity with nociception and pain. And, at last, there seemed to be proportional relationships between the amount of matrix activity and pain. And in the move from the periphery to the brain, a common motivation has been: "Change function in the pain matrix and the pain will also change". As part of this move, and based on strong scientific evidence, it has long been (rightly) said: "Nociceptor activity and pain are not the same thing". So the remainder of the evidence went to the brain. However, a new study again raises the question: "What pain matrix?" Salomons et al (2016) studied nociception, pain and matrix activity in healthy subjects who could feel pain and compared the activity in the alleged pain matrix in people who could not (congenital insensitivity to pain). METHODS Subjects were of two groups: Group 1. Healthy and who could feel pain, Group 2. Subjects who could not feel pain (congenital insensitivity to pain). Because of their lack of pain, these people often have short lives because they are unable to respond to nociception related to injury, illness and pathology. A noxious stimulus was applied to the dorsum of the hand of all subjects and measurements taken of responses in the "pain matrix" with fMRI. Data were collected on intensity of "sensation" (0-10) and intensity of "pain" (0-10). A meta-analysis from hundreds of pain and brain imaging studies was performed to establish the requirements for pain matrix activity, such that the evidence for these areas constituting the pain matrix was as good as it gets. Among others, the thalamus, anterior cingulate cortex and insula were key areas. Los Angeles Neurodynamics Courses Fix Your Own Back |
RESULTS
Both groups did not differ significantly in relation to intensity of "sensation" (4.6 vs 4.4). The healthy subjects (who could feel pain) reported pain and its intensity to be 3.2. Not surprisingly, the group with congenital insensitivity to pain reported no pain. The surprise was that activity in the "pain matrix" in both groups was the same. DISCUSSION This study suggests that the "pain matrix" is not specifically a pain matrix. Just as: "Nociceptor activity and pain are not the same", also may now be said: "Nociceptive (pain matrix) activity in the brain and pain are not the same". As discussed by Professor Waxman in the ensuing editorial, instead it may be a matrix for nociception and other functions that have the quality of 'salient', or what is motivationally important (Legrain et al 2011). These could relate to many things such as a sudden loud noise, fear, threat, need to focus on something, an intense emotion, something that attracts our attention. In the past it was said "Since pain and nociceptor activity are not the same thing, don't focus on the body and don't give pain anatomy or biology. Treat the brain because that's where the real action is". Now it appears that the pain matrix attracts the same intellectual, ethical and clinical challenges that nociception did. For a time, nociception attributed pain to anatomy and biology, much to the chagrin of those who disagreed. But, as the matrix was allocated brain areas and mechanisms, pain was again given anatomy and biology. This is not for one moment to say that we should retreat from the brain because development in this area is likely to be key to long term pain management and treatment. As a clinician treating pain and applying it to the brain, some of the best responses to certain problems can be effected through a top down approach. But it seems pain is, yet again, more complex than we thought and the shortfall in our understanding of nociception and pain in our patients remains as large as ever. IMPLICATIONS FOR CLINICAL PRACTICE Psychiatrists have for a long time been saying "You can't image pain because it's an experience unique to the individual". This may still be the case, at least for now. Educating patients about their brain and pain continues to be difficult because the exact relations between the two remain unknown. General theories as to how pain occurs remain elusive and, even though ongoing study in this area is greatly needed, the uniqueness of pain continues to prevail. N=1 remains a very important statistic. REFERENCES Salomons T, Iannetti G, Liang M, Wood J 2016 The “Pain Matrix” in pain-free individuals. Journal of the American Medical Association (JAMA) Neurology 73 (6): 755-756 Legrain V, Iannetti G, Plaghki L, Mouraux A 2011 The pain matrix reloaded: a salience detection system for the body. Progress in Neurobiology 93 (1): 111-124 |