Acute Lumbar Radiculopathy: Is it Possible to Reduce Force on the Nerve Root?

Introduction
Many clinicians have been confronted with trying neural mobilisation for the acute painful nerve root problem to find that it often provokes. When we consider the mechanisms, the offending mechanism is most commonly excessive force (pressure) on the root by protruding invertertebral disc (see below). It is intriguing that, in one of the most recognisable acute pain syndromes where excessive force is a key, a treatment approach is to apply more force via mobilising the nerve root. Maybe adaptive mechanisms are stimulated whereby some patients are helped, but here we explore another way. This short discussion focuses on the question: "Can we, at least transiently, reduce force on the lumbar nerve root for acute radicular pain?" This necessitates an analysis of the research where force in the lumbar intervertebral foramen (IVF) has been measured with pressure transducers in patients with disc protrusion and lumbar radiculopathy during different spinal manoeuvres. Also the possibility of correlations existing between certain pressure changes and clinical signs has been investigated. Also required is consideration of what this produces in the nerve root itself in terms of biological markers that integrate pressure and intraneural blood flow with the gold standard of diagnosis - electrophysiology. What Happens to Pressure in the Foramen in Patients with Radiculopathy Due to Disc Protrusion? Here is a profile of the pressures in the IVF in such patients. 1. Those with a contralateral list have approximately double the pressure of those who do not (Takahashi et al 1999):
2. Those with neurological impairment also have higher IVF pressure than those who do not (Takahashi et al 1999):
3. Pressure on the nerve root produces reduced blood flow and correlates with electrophysiological impairment (muscle action potentials, latency and amplitude; Takamori et al 2011). Michael Shacklock's upcoming presentations in the US
Chicago Denver, International Spine and Pain Institute Detroit (1 day masterclass, Team Rehab PT) Seattle Los Angeles Columbus, OH San Francisco, Stanford University |
Does Pressure on the Nerve Root Change with Lumbar
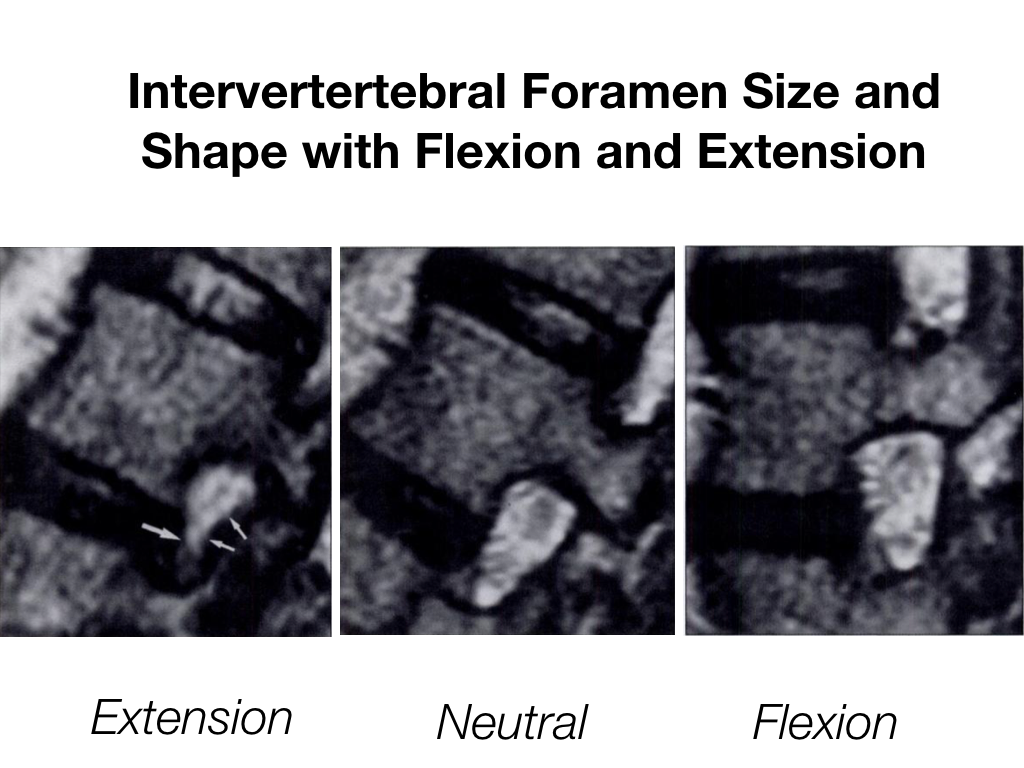
Movements? Yes - pressure in the foramen reduces by as much as 53% from lumbar extension to flexion and 33.8% from neutral to flexion and this produces improvements in nerve root blood flow and electrophysiology in patients with radiculopathy (Morishita et al 2006). This does not take into account contralateral lateral flexion which also adds to foramen opening (Nowicki et al 1996, Schmid et al 1999, Fujiwara et al 2001), so the above values are likely to be conservative. Below is a radiological example of the lumbar IVF in different lumbar positions (from Schmidt et al 1999). A key question is whether this produces longer or 'carry-over' effects that outlast the duration of the manoeuvre.
Maybe there are patients who do better when we open the foramen instead of mobilising the nerve root, particularly in the acute severe phase. SUMMARY 1. Patients with sciatica and lumbar radiculopathy due to disc protrusion have increased pressure on their nerve root which produces ischaemia and electrophysiological impairment. 2. People with trunk list and neurological impairment have higher pressures than people who do not have list or neurological compromise. 3. Flexion and contralateral lateral flexion open and reduce pressure in the foramen by 30-50% and this correlates with early improvement in nerve root blood flow and electrophysiology. 4. What remains interesting is whether such rapid changes show a carry-over effect into patient outcomes. |
REFERENCES
Fujiwara A, An H, Lim T, Haughton V 2001 Morphologic changes in the lumbar intervertebral foramen due to flexion-extension, lateral bending, and axial rotation: an in vitro anatomic and biomechanical study. Spine 26 (8): 876-882
Morishita Y, Hida S, Naito M, Arimizu J, Matsushima U, Nakamura A 2006 Measurement of the local pressure of the intervertebral foramen and the electrophysiologic values of the spinal nerve roots in the vertebral foramen. Spine 31 (26): 3076 –3080
Nowicki B, Haughton V, Schmidt T, Lim T, An H, Riley L 3rd, Yu L, Hong J 1996 Occult lumbar lateral spinal stenosis in neural foramina subjected to physiologic loading. American Journal of Neuroradiology 17 (9): 1605-1614
Schmid M, Stucki G, DueweII S, Romanowski B, Hodler J 1999 Changes in cross-sectional measurements of the spinal canal and Intervertebral foramina as a function of body position: studies on an open-configuration system. American Journal of Radiology 172: 1095-1102
Takahashi K, Shima I, Porter R 1999 Nerve root pressure in lumbar disc herniation. Spine 24 (19): 2003-2006
Takamori Y, Arimizu J, Izaki T, Naito M, Kobayashi T 2011 Combined measurement of nerve root blood flow and electrophysiological values: intraoperative straight-leg-raising test for lumbar disc herniation. Spine 36 (1): 57-62
Fujiwara A, An H, Lim T, Haughton V 2001 Morphologic changes in the lumbar intervertebral foramen due to flexion-extension, lateral bending, and axial rotation: an in vitro anatomic and biomechanical study. Spine 26 (8): 876-882
Morishita Y, Hida S, Naito M, Arimizu J, Matsushima U, Nakamura A 2006 Measurement of the local pressure of the intervertebral foramen and the electrophysiologic values of the spinal nerve roots in the vertebral foramen. Spine 31 (26): 3076 –3080
Nowicki B, Haughton V, Schmidt T, Lim T, An H, Riley L 3rd, Yu L, Hong J 1996 Occult lumbar lateral spinal stenosis in neural foramina subjected to physiologic loading. American Journal of Neuroradiology 17 (9): 1605-1614
Schmid M, Stucki G, DueweII S, Romanowski B, Hodler J 1999 Changes in cross-sectional measurements of the spinal canal and Intervertebral foramina as a function of body position: studies on an open-configuration system. American Journal of Radiology 172: 1095-1102
Takahashi K, Shima I, Porter R 1999 Nerve root pressure in lumbar disc herniation. Spine 24 (19): 2003-2006
Takamori Y, Arimizu J, Izaki T, Naito M, Kobayashi T 2011 Combined measurement of nerve root blood flow and electrophysiological values: intraoperative straight-leg-raising test for lumbar disc herniation. Spine 36 (1): 57-62